Intro.
Factors affecting Contractility can be either intrinsic, extrinsic, or other factors relating to ion concentrations etc…
Contractility (cont.)
Factors affecting contractility can be:
Intrinsic factors.
Preload. (End Diastolic Volume.)
- It is the load that determines the initial length of the resting muscle before it contracts.
- Increased EDV means that the muscle will begin contracting from a longer position, causing a stronger contraction. (Length-Tension relationship.)
- This is the basis of the Frank-Starling law AKA Heterometric-Autoregulation of the heart which states that: “Within reason, the force of myocardial contraction is proportional to its initial length.” This mechanism’s significance is:
- Normal heart rate matches ventricular output to venous return.
- Increased aortic pressure decreases stroke volume of left ventricle causing an increase in the next beat’s EDV causing a more powerful contraction.
- It is the main mechanism regulating pumping capacity of the heart.
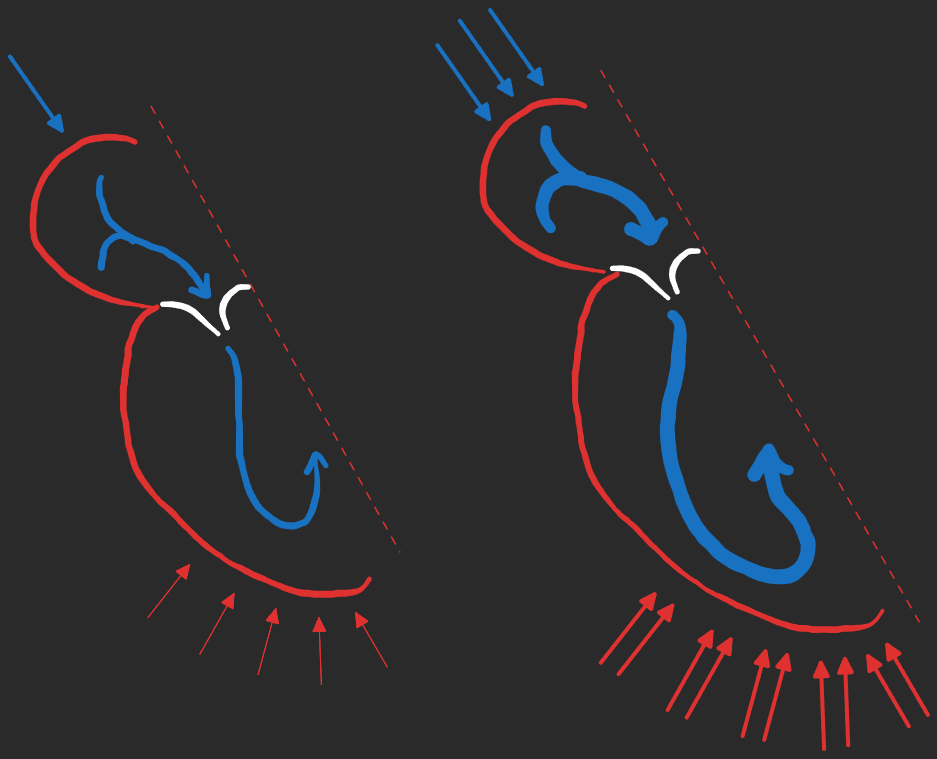
Afterload. (Aortic pressure, Arterial rigidity, Blood viscosity.)
- It is the load that the muscle fibers face when they contract.
- Increased AP, AR, or BV means that the velocity of muscle shortening is reduced.
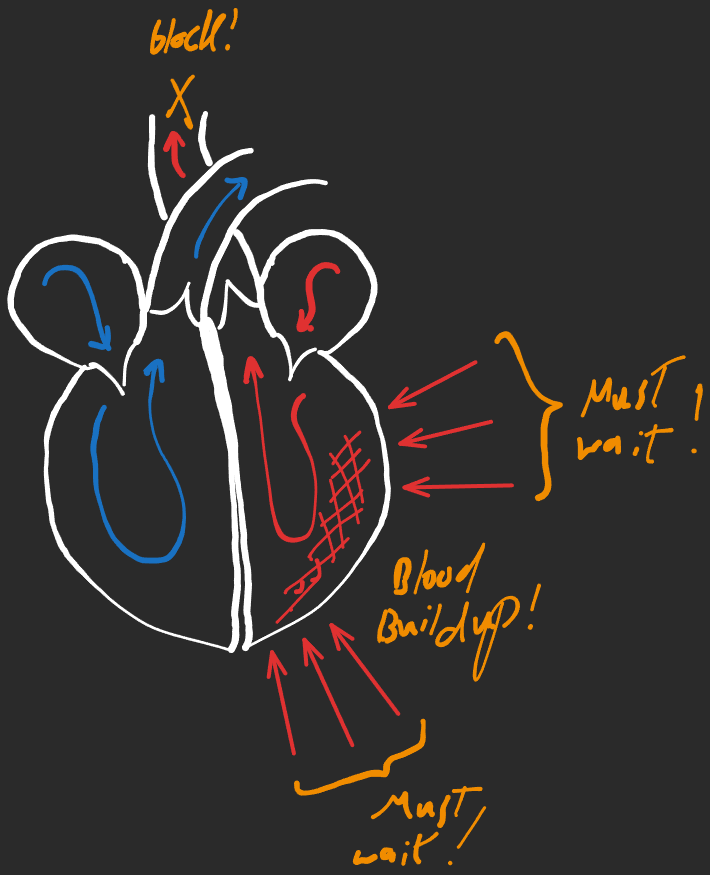
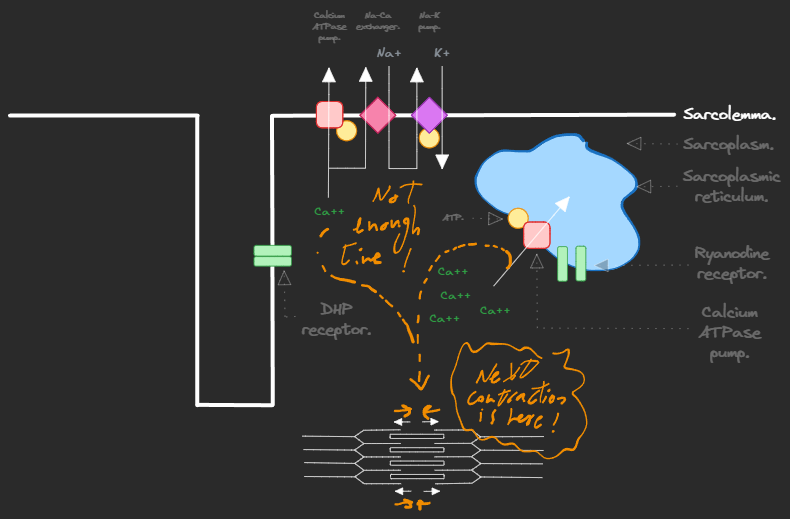
Heart rate.
- Increased HR will increase the force of myocardial contractility due to build up of intracellular Ca++.
Extrinsic factors.
Nervous factors.
- Sympathetic -⇒ + inotropic.
- Vagal -⇒ - inotropic.
Physical factors.
- Heating.
- Moderate rise in temperature -⇒ + contractility.
- Excessive rise in temperature -⇒ - contractility.
- Cooling -⇒ - contractility.
Chemical factors.
- Hormones.
- Catecholamines -⇒ + inotropic.
- Thyroid hormones -⇒ + inotropic. (T4 -⇒ T3 acting as a -agonist.)
- Blood gases.
- Moderate hypoxia or moderate hypercapnia -⇒ + inotropic.
- Severe hypoxia -⇒ - inotropic.
- Ions.
- Hyperkalemia -⇒ - inotropic.
- Hypercalcemia -⇒ + inotropic.
- Acidosis (increased H+) -⇒ - inotropic.
- Alkalosis (decreased H+) -⇒ + inotropic.
- Toxins -⇒ - inotropic.
Conductivity.
It is the ability of the heart to conduct the excitation waves to all its parts.
Once the SA node (pacemaker) sends an impulse to contract, the AP travels down the internodal pathway which is composed of 3 bundles of conductive cardiac muscle cells between the SA and AV nodes (vel. = 1m/s) At the AV node (vel. = 0.05 m/s) the AP is delayed by 0.2 seconds, this allows for:
- Spread of excitation waves to the auricles, allowing for more ventricular filling.
- Protection of the ventricles from high auricular rhythm.
Then, the AP is transferred to the AV bundle (vel. = 3~5 m/s) which transfers it to the ventricular muscle itself (vel. = 0.5 m/s) which is slower to allow time for the larger ventricular muscle to contract.
Excitability.
It is the ability of cardiac muscle to respond to stimulus by contracting.
ARP. A complete loss of excitability, is very long in cardiac muscle (occupies all systole.) Corresponds to phase 0, phase 1, and phase 2 of AP. Since ARP is so long, it prevents heart tetanization. RRP. A partial loss of excitability, occupies all diastole. Corresponds to phase 3 of AP. Supernormal period. An overexcitability of cardiac muscle. Also called the “Dangerous period”.