Intro.
The properties of the heart include auto-rhythmicity, excitability, conductivity, and contractility.
Auto-rhythmicity.
Automaticity + Rhythmicity means that the heart can regularly and rhythmically self-excite. The mechanism is as follows:
Mechanisms of auto-rhythmicity.
- The heart relies on self-generated myogenic impulses instead of the more typical neurogenic ones.
- These impulses are generated by the SA node AKA the “pacemaker” of the heart. (all parts of the heart are auto-rhythmic, for ex.: AV node is the 2ry pacemaker, Purkinje systems is the 3ry pacemaker, Cardiac muscle cells are the 4ry pacemaker.)
How is the pulse generated?
- Influx of Na+ through funny Na+ channels initiates depolarization from -60mv.
- Influx of Ca++ through T (Transient) Ca++ channels continues depolarization.
- Influx of Ca++ through L (latent) Ca++ channels further depolarizes the cell until threshold is reached.
- Influx of Ca++ continues through the L channels causing membrane potential to reach +10mv at which they become inactivated and close. At the same time, K+ channels open allowing K+ efflux and membrane potential starts to drop.
- Influx of Na+ through funny Na+ channels which starts the next action potential.
Factors affecting rhythmicity.
Cardiac innervation.
Can be summed up in:
- Sympathetic stimulation.
- Causes tachycardia.
- Decreases SA node permeability to K+ leading to less K+ being available for repolarization causing hyper-excitability of SA node (increased slope) and increased HR.
- Parasympathetic stimulation.
- Causes bradycardia.
- Increases SA node permeability to K+ leading to more K+ being available for repolarization causing hypo-excitability of SA node (decreased slope) and decreased HR.
Ionic concentrations.
Mostly regarding Na+ and K+ concentrations:
- K+ conc.:
- Decreased K+ ⇒ Tachycardia.
- Increased K+ ⇒ Bradycardia.
- Na+ conc.:
- Decreased Na+ ⇒ inability to initiate impulse.
- Increased Na+ ⇒ initiates impulse, but cant maintain it.
Physical factors.
- Cooling. ⇒ Bradycardia.
- Heating. ⇒ Tachycardia.
- Exercise. ⇒ Tachycardia.
- Endurance athletes. ⇒ Resting Bradycardia.
Chemical factors.
- Thyroid hormones & catecholamines. ⇒ Tachycardia.
- Acetylcholine. ⇒ Bradycardia.
- Hypoxia. ⇒ Bradycardia.
(Bradycardia = reduced rhythmicity. Tachycardia = increased rhythmicity.)
Electrical activity of contractile muscle fibers.
Contractile cells demonstrate a much more stable resting phase than conductive cells at approximately −80 mV for cells in the atria and −90 mV for cells in the ventricles.
AP of contractile muscle fibers.
- Na+ channels open allowing influx of Na+ ions, raising membrane potential to +30 mV.
- At 30 mV, Na+ cannels close and K+ channels open allowing outflux of K+ ions.
- Repolarization is slow due to opening of slow Ca++ channels allowing slow influx of Ca++ ==opposing the outflux of K+, causing a plateau==.
- Once membrane potential reaches 0 mV Ca++ channels close, causing rapid repolarization to RMP due to electrically unopposed K+ outflux.
- ==Na-K pumps activate to restore Na+ and K+ concentration==.
(Phases start from 0, so number 1 is actually phase-0, number 2 is actually phase-1, and so on.)
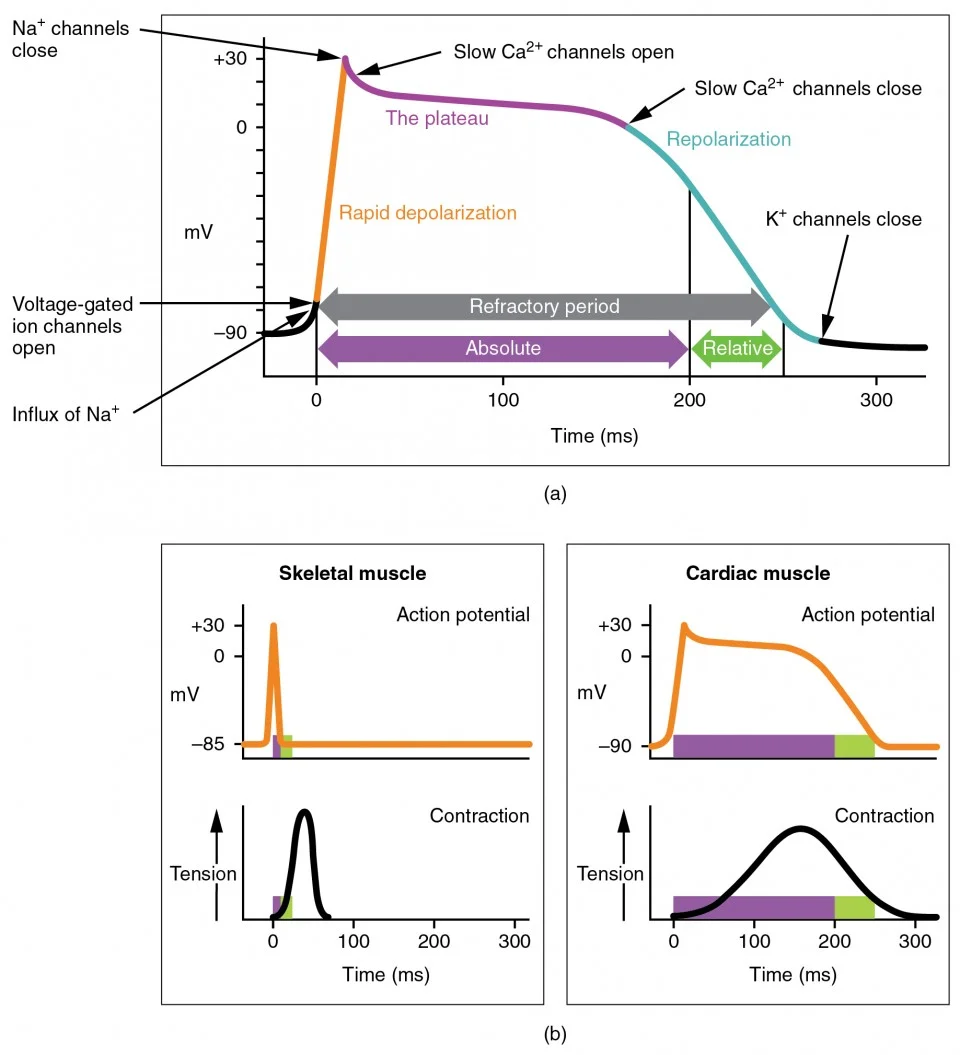
Why is the plateau important?
- The plateau prolongs ARP of cardiac muscle which prevents Tetanization of the heart.
- The Ca++ influx during the plateau provides 20% of the Ca++ required for contraction.